Since ancient times, the biology of women has been seen from the male model. At that time, there was a vision of the single sex, that is, there was only one sex, which was man, and women were inferior versions of this model.
Hundreds of myths were maintained over time. And although in the Middle Ages, Andreas Vesalius modified the vision of the anatomy described by Galen, what didn’t change was the vision towards bodies that didn’t correspond to the male sex. Vesalius continued to describe women’s bodies as men’s but in reverse, that is, reaffirming those beliefs that Aristotle already had years ago. Women were marked by their anatomical differences from men and this made them medically defective.
In the 17th century there was a professionalization of medical science. But it was not until the 18th century, when the vision of the dual body was established, now that two sexes were differentiated: men and women. Leaving out of that classification other realities such as intersex people.
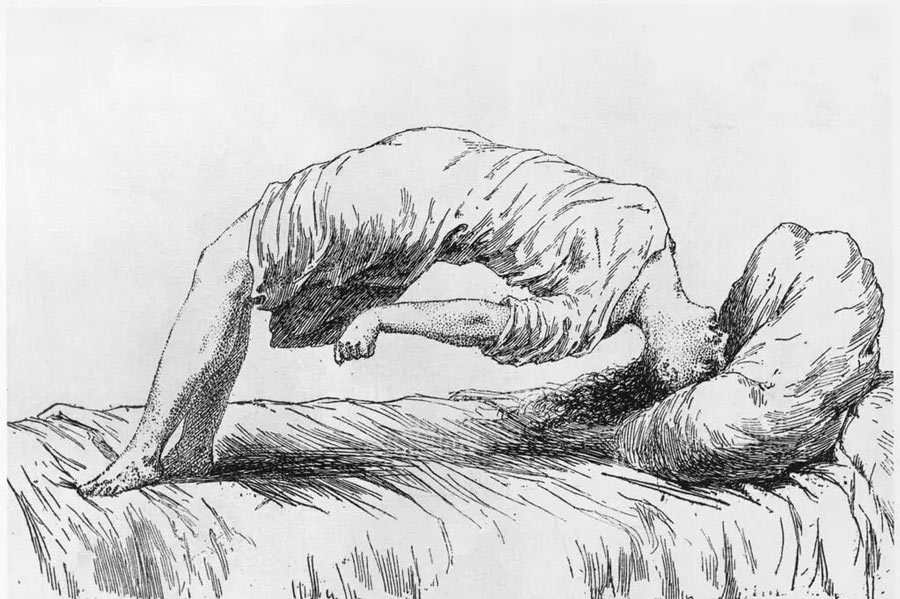
“Women’s health” was taken for granted to refer to reproductive health, including childbirth care, contraception, abortion, uterine cancer, and other specifically female diseases. For centuries, women were subject to myths about their “curious biology”, with pathologies that seemed inexplicable, or always subject to menstruation or hysteria.
Many of her afflictions were reduced to hysteria, that diagnosis that accompanied women with “nervous problems” for centuries, which in the Middle Ages could lead you to the stake accused of witchcraft or later in the 19th century to a sanatorium for getting out of the norm.
And today we find pathologies that are frequent and that affect only or in a greater proportion women whose exact origin is unknown, such as endometriosis or fibromyalgia. In fact, when these types of “unexplained” illnesses began to be diagnosed at the beginning of the 20th century, it was easier for doctors to continue saying that they were caused by nerves or hysteria than to admit that the cause wasn’t known.
The case of fibromyalgia affects both women and men in a ratio of 9:1. It is understood as a neuropathic pain syndrome caused by stress, which can open new paths for gender relations. It is underdiagnosed, however today from scientific research many efforts are being made to find the cause. New studies show it’s because women have seven times less serotonin in their brains. Other theories say that it is caused by biochemical changes in the body and may be related to hormonal changes or menopause.
Certain knowledge gaps in science are not always just a coincidence. The fact that for so long women were removed from scientific research and subjected to so many myths about their bodies, has harmed the attention that has been given to many pathologies.
References:
Cleghorn, E. (2021). UNWELL WOMEN. A Journey Through Medicine and Myth in a Man-Made World. The Orion publishing group.
García & Pérez. (2018). Las ‘mentiras’ científicas sobre las mujeres. Catarata.
Martínez-Lavín, M. (2021). Fibromyalgia in women: somatisation or stress-evoked, sex-dimorphic neuropathic pain. Clin Exp Rheumatol, 39(2), 422-5.
Rich-Edwards, J. W., Kaiser, U. B., Chen, G. L., Manson, J. E., & Goldstein, J. M. (2018). Sex and gender differences research design for basic, clinical, and population studies: essentials for investigators. Endocrine reviews, 39(4), 424-439.
Shannon, G., Jansen, M., Williams, K., Cáceres, C., Motta, A., Odhiambo, A., … & Mannell, J. (2019). Gender equality in science, medicine, and global health: where are we at and why does it matter?. The Lancet, 393(10171), 560-569.